Technologies
Pulse Oximetry
Masimo SET® Overcomes Limitations of Conventional Pulse Oximetry
Masimo SET®, or Signal Extraction Technology®, is the industry-leading, clinically proven pulse oximetry technology that enables accurate monitoring of oxygen saturation and pulse rate for greater visibility of oxygenation. Masimo SET® measures accurately through motion and low perfusion, across patient populations and skin pigmentations.1
Over 100
studies
have shown that Masimo SET® outperforms other pulse oximetry technologies.1
200+ million
patients
are monitored by Masimo SET® pulse oximetry each year.2
All top 10
U.S. hospitals
as ranked in the 2024 Newsweek World’s Best Hospitals listing use Masimo SET® as their primary pulse oximetry technology.3
Unrivaled
SpO2 accuracy
with RD SET® pulse oximetry sensors, achieved through continued innovation.4
The Basics of Pulse Oximetry
What Is Pulse Oximetry?
Pulse oximetry is a noninvasive method of measuring arterial oxygen saturation and pulse rate.
- Oxygen Saturation is the percentage of hemoglobin that is bound to oxygen (O2) and is being transported for delivery to various parts of the body.5
- Pulse Rate (PR) is the number of heart beats per minute.6
In the past, oxygen saturation measurements could only be obtained invasively through laboratory tests that measured the oxygen in an arterial blood sample (SaO2), and pulse rate was obtained through auscultation with a stethoscope.
Why Is Pulse Oximetry Important?
Oxygen plays a critical role in cellular metabolism and oxygen deprivation can result in serious consequences and even death.7,8 Therefore, it is necessary to monitor the levels of oxygen in the blood as well as the rate at which it is being transported throughout the body.
- Normal oxygen saturation is considered to be between 95% and 100%.6
- Oxygen saturation below 90% is considered low, or hypoxemic, saturation.6
How Does Pulse Oximetry Work?
All pulse oximeters analyze the pleth, a pulse wave originating from the heart and traveling to the measurement site, such as a fingertip or another tissue. By emitting and detecting light at various frequencies through the site, the pulse oximeter measures the amount of light absorption and uses that to provide relevant patient data based on signal processing and algorithmic analysis.
- Oxygen saturation from pulse oximetry (SpO2) is measured by analyzing the relative amount of red and infrared light absorbed as it fluctuates with the cardiac cycle.9
- Pulse rate is measured by counting the number of arterial pulses over a specified time.6
Common Limitations of Pulse Oximetry
Some pulse oximetry devices may not distinguish the true arterial signal from noise, for example, caused by the movement of venous blood.

Motion
Many manufactured devices only provide accurate readings when a patient is not moving10 – making treating babies very challenging.11

Low Perfusion
Conventional pulse oximeter devices struggle to deliver accurate readings in people with low perfusion.12

Skin Pigmentation
Some pulse oximetry devices tend to overestimate arterial oxygenation in darker skin, negatively impacting their ability to detect hypoxemia.13
Therefore, conventional pulse oximeters may lead to high rates of false alarms and failed measurements when used in challenging conditions, such as on patients with low perfusion or during motion.10
Masimo and the Birth of SET® Pulse Oximetry
Joe Kiani, Founder and CEO of Masimo, established the company precisely to address the common limitations of pulse oximeters through the use of adaptive signal processing. The solution, Masimo SET® Measure-through Motion and Low Perfusion™ pulse oximetry, was born.
Since its introduction, Masimo SET® has been shown in more than 100 independent and objective studies to outperform other pulse oximetry technologies.1 Today, Masimo SET® is used at top hospitals worldwide to monitor more than 200 million patients each year.2,3

How Masimo SET® Works
All pulse oximeters analyze red and infrared light that is absorbed by the application site and translate it to pulse oximetry values displayed on the screen. Masimo SET® further utilizes the following techniques to provide accurate measurements:
- SET® employs advanced signal processing systems – including parallel engines and adaptive filters.
- Masimo SET® sensors and cables are designed to shield themselves from external electromagnetic and ambient light interference to provide optimal performance.
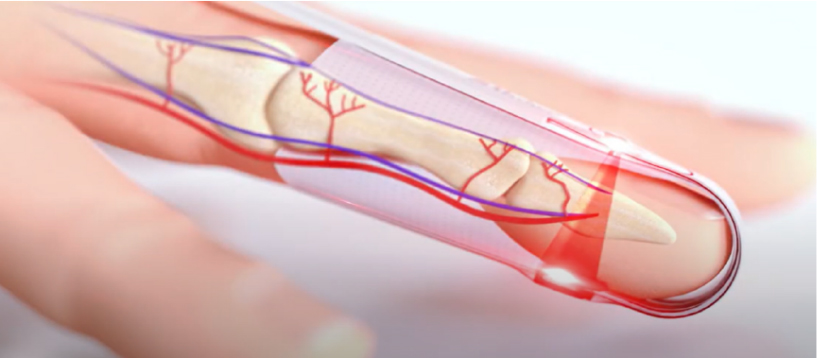
These two factors in combination allow clinicians to measure oxygen saturation and pulse rate accurately in a variety of scenarios, including during motion, in low perfusion, and across varying skin pigmentation.
Masimo SET®: Accuracy for All
Masimo SET® technology provides accurate readings across all patient populations and clinical settings.
All Patient Populations
- Masimo SET® can measure accurately on people of all ages, from premature babies to geriatric adults.1
- Masimo offers sensors for patients of all weights, including for babies weighing less than 1 kg.
All Skin Pigmentations
- Masimo SET® has been designed, calibrated, and validated using nearly equal numbers of dark- and light-skinned subjects.13
- Peer-reviewed studies have shown that Masimo SET® pulse oximetry works accurately in varying skin pigmentation.12-14
All Clinical Settings
Masimo SET® is used in all care areas of the hospital and beyond.
In the Hospital
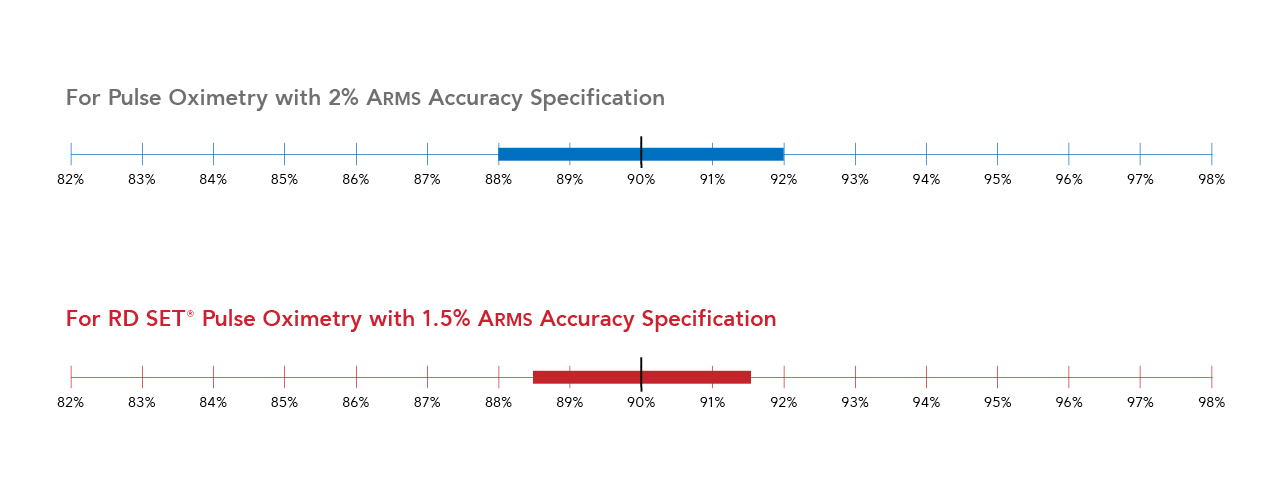
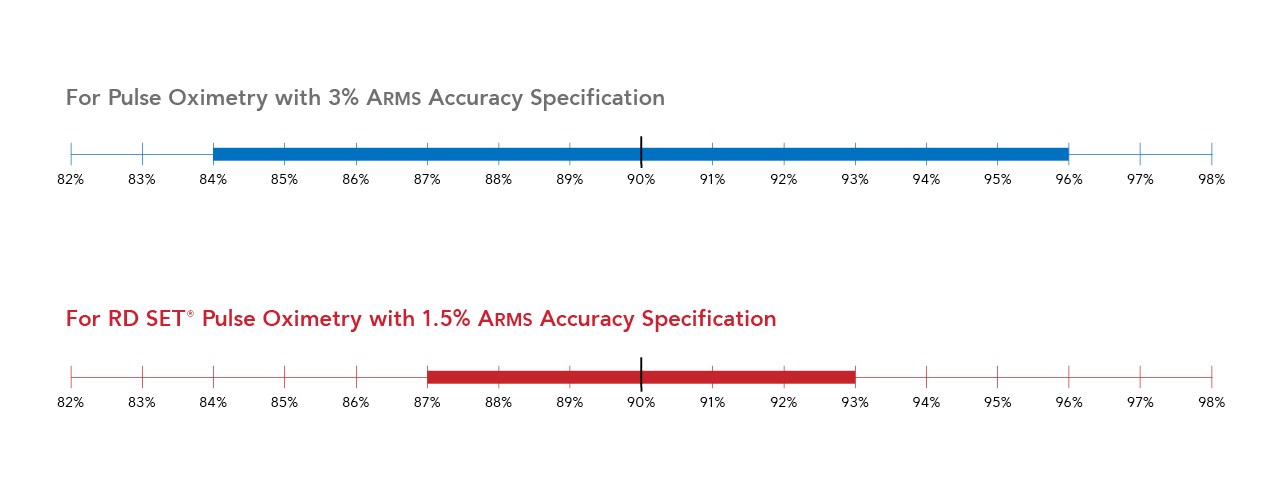
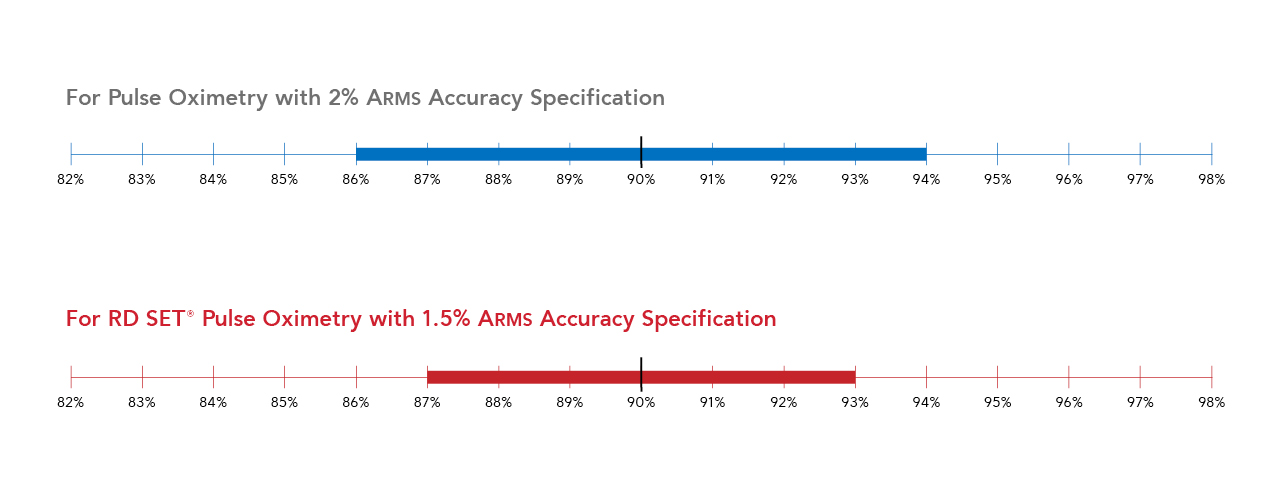
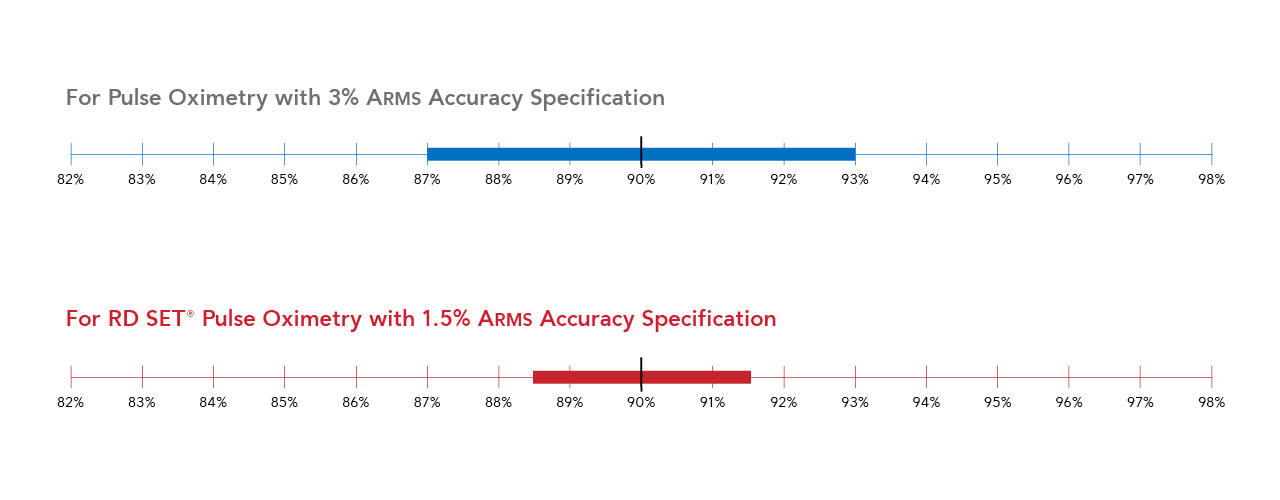
What Do ARMS* Accuracy Specifications Mean for Patient Care?
Accuracy Root Mean Square error (or ARMS) is an established measure of performance.
- ARMS is used by regulatory agencies, such as the FDA, to determine how accurately a pulse oximeter performs.15
- For oxygen saturation, ARMS accuracy is a statistical representation of the estimated difference between SpO2 measurements and reference arterial blood gas (SaO2) readings.
- Approximately two-thirds (68%) of the SpO2 values are expected to fall within ± ARMS of the reference measurements.
| Condition | SpO2 ARMS Specification (70-100%) | Pulse Rate ARMS Specification (25-240 bpm) |
|---|---|---|
| No Motion |
1.5% |
3 bpm |
| Motion |
1.5% |
5 bpm |
| Low Perfusion |
2% |
3 bpm |
Masimo RD SET sensors outperform the industry-wide SpO2 accuracy specification of 3% ARMS.4,15
ARMS Accuracy Simulation
Click on the options below to see the expected SpO2 range for RD SET® and industry-wide pulse oximetry when the true oxygen saturation is 90%.
Condition
Expected SpO2 Range
The expected SpO2 range is:
Impact to Workflow Efficiency
Masimo SET® provides false alarm reduction, better true alarm detection, decreased sensor usage, compatibility with a variety of third-party monitors, and tailored settings for various clinical needs.
False Alarm Reduction
The accuracy of Masimo SET® pulse oximetry leads to fewer false alarms and better true alarm detection,10 reinforcing clinician confidence in measurements for all types of patients.
- Switching from sensors with 3% ARMS to 1.5% ARMS SpO2 accuracy specifications in motion theoretically implies a more than 4-fold decrease in false alarms when the SpO2 alarm threshold is set to 90% and the true value is 92% (SaO2).16
- In a clinical setting, researchers have found that “Masimo SET® recorded markedly fewer false SpO2 and PR alarms and identified more true hypoxic and bradycardic events in neonates” when compared with other pulse oximeters.11
See additional advantages of Masimo SET® performance compared to Nellcor OxiMax
Better True Alarm Detection
In a study during challenging conditions of motion and low perfusion:
- Competitor pulse oximetry technology demonstrated 43% missed true alarms while Masimo SET® demonstrated 3% (93% reduction).10
- There was a 82% reduction in false alarms between competitor technology and Masimo SET® (28% and 5%, respectively).10
See a side-by-side video comparing Masimo SET® and Nellcor OxiMax in motion and low perfusion
Decreased Sensor Usage
The ability to measure through motion and low perfusion in critically ill patients with Masimo SET® digit sensors enables accurate pulse oximetry readings and may also reduce the need for clinicians to resort to more expensive alternate site options like the forehead or ear sensor.
- Less than 1% of Masimo SET® sensors used in hospitals are placed on alternate measurement sites (like the forehead or ear), because clinicians rely on Masimo digit sensors.16
- A peer-reviewed study of 12 hospital units found a 60% reduction in single-patient-use sensors by retaping with Masimo replacement tapes, instead of reprobing, allowing clinicians to “recheck and reposition sensor sites with minimal cost and difficulty.”17
See a real-world example of the impact of Masimo replacement tapes on sensor usage

Compatibility with a Variety of Third-party Monitors
In addition to Masimo’s comprehensive device portfolio, Masimo SET® is also integrated in over 250 third-party monitors from other leading patient monitoring equipment manufacturers, facilitating a more seamless workflow for clinicians.18
See the list of third-party companies whose monitors can be enabled with Masimo SET® technology
Tailored Settings for Various Clinical Needs
Masimo devices provide settings, like averaging time and sensitivity modes, that are customizable to meet the needs of the particular clinical situation.
- Masimo specialty sensors that automatically use relevant settings to obtain fast readings in situations such as trauma and newborn resuscitation are also available.
- In a study comparing pulse oximeters in newborns during resuscitation using the highest sensitivity and two-second averaging setting, Masimo SET® was found to be over 45 seconds faster (mean difference) than competitor technology to show stable readings of both SpO2 and pulse rate.19
See the Masimo specialty sensor portfolio that may help improve your clinical workflow
Products for All Patients and Needs
Masimo SET® technology and pulse oximetry sensors are available for all patient populations, including neonates, infants, children, and adults.
In addition, Masimo SET® technology is available on a wide variety of multi-parameter, bedside, handheld, and fingertip pulse oximeters.
Radius PPG®
Tetherless Pulse Oximetry
Continuous monitoring on the move with Masimo SET® measure-through motion and low perfusion™ technology
RD SET®
Sensors and Cables
Lightweight, low-profile SET® sensors with best-in-class accuracy specifications
Masimo Sensors Offer a Unique Array of Breakthrough Parameters
In addition to SpO2 and PR, all Masimo SET® products provide a noninvasive measure of peripheral perfusion with the perfusion index (Pi) parameter. Studies have evaluated Pi’s clinical utility, for example, in critical congenital heart disease (CCHD) screening in infants.20-22
Masimo SET® Parameters
Foundational Monitoring Available on All SET® Sensors and Devices
Oxygen Saturation†
Pulse Rate†
Perfusion Index
At Masimo, our innovative technologies also go beyond basic pulse oximetry to include a unique array of advanced parameters (noted in red circles) obtained through rainbow® multi-wavelength (4+ LEDs) sensors.
By utilizing these parameters, clinicians can gain visibility to patients’ fluid responsiveness status,‡ respiration rate, oxygenation in the moderate hyperoxic range, hemoglobin concentration, and dyshemoglobin levels.
Upgradable Parameters
Enhanced Monitoring Available on Compatible Sensors and Devices
Sustainability and Health Equity
At Masimo, we are focused on providing fair and equal access to healthcare by ensuring that our pulse oximetry sensors perform accurately on all skin tones,12,13 while also prioritizing sustainability.
We understand that the materials we use and the products we manufacture — including single-patient-use sensors – can have a profound impact on the environment. From sensor design to disposal, Masimo uses materials that are less wasteful and more environmentally friendly without compromising quality or performance.
Masimo RD Sensors: Designed for Sustainability
Masimo RD single-patient-use sensors have become the first ever pulse oximetry products to be recognized with the coveted Greenhealth Approved seal, a designation that is only granted to products that meet specific sustainability criteria.
RD single-patient-use sensors:
- Reduce waste by 84% when compared to cable-based sensors.16
- Achieve zero waste to landfill through Masimo’s sensor recycling program.
- Allow for “reprocessing at the bedside” with replacement tapes.
- Meet the chemical criteria of Health Care Without Harm.
- Have eliminated over 2,000 metric tons (MT) of material between 2016 and 2023 through material changes.16
Masimo SET® Clinical Evidence
The impact of Masimo SET® technology has been demonstrated in a variety of peer-reviewed studies.
-
CLINICAL EVIDENCE
Improved Outcomes in Children
“Can Changes in Clinical Practice Decrease the Incidence of Severe Retinopathy of Prematurity in Very Low Birth Weight Infants?”
Chow LC et al. Pediatrics. 2003;111(2):339-45.
- The results indicated that “The incidence of ROP [retinopathy of prematurity level] 3 to 4 at this center decreased consistently in a 5-year period from 12.5% […] to 2.5%…”23
“Prevention of Retinopathy of Prematurity in Preterm Infants Through Changes in Clinical Practice and SpO2 Technology”
Castillo et al. Acta Paediatr. 2011 Feb;100(2):188-92.
- The authors concluded that “In a large group of inborn infants < 1250 g, a change in clinical practice in combination with pulse oximetry with Masimo SET®, but not without it, led to significant reduction in severe ROP [retinopathy of prematurity] and need for laser therapy.”24
-
CLINICAL EVIDENCE
Improved Outcomes in Adults
“Inpatient Respiratory Arrest Associated with Sedative and Analgesic Medications: Impact of Continuous Monitoring on Patient Mortality and Severe Morbidity”
McGrath S et al. J Patient Saf. 2021; 17(8):557-561.
- The study results indicated that “Of 111,488 patients in units with surveillance monitoring available, none died or were harmed by opioid-induced respiratory depression when surveillance monitoring [with Masimo SET®] was in use.”25
“Surveillance Monitoring Management for General Care Units: Strategy, Design, and Implementation”
McGrath S et al. Jt Comm J Qual Patient Saf. 2016; 42(7): 293-302.
- The study results indicated that “Improvements in clinical outcomes [included a] reduction of unplanned transfers by 50% and reduction of rescue events by more than 60%…”26
-
CLINICAL EVIDENCE
Accuracy in Challenging Conditions
“Performance of Three New-generation Pulse Oximeters During Motion and Low Perfusion in Volunteers”
Shah et al. J Clin Anesth. 2012;24(5):385-91.
- The authors concluded that “Masimo [Radical-7®] had higher SpO2 sensitivity and specificity than Nellcor N-600 and Datex-Ohmeda TruSat during conditions of motion and induced low perfusion in this volunteer study.”10
“Avoiding Hyperoxemia During Neonatal Resuscitation: Time to Response of Different SpO2 Monitors”
Baquero H et al. Acta Paediatr. 2011 Apr;100(4):515-8
- The authors concluded that “The time to a reliable reading obtained simultaneously in neonatal critical situations differs by the type of the pulse oximeter used, being significantly faster with Masimo Signal Extraction Technology. This may permit for better adjustments of inspired oxygen, aiding in the prevention of damage caused by unnecessary exposure to high or low oxygen.”19
“Accuracy of Pulse Oximeters Intended for Hypoxemic Pediatric Patients”
Harris B. et al. Ped Crit Care Med. 2016;17(4):315-20.
- The authors concluded that “The Masimo Blue sensor has improved accuracy at saturations 75-85% versus [other] sensors.”27
-
CLINICAL EVIDENCE
Accuracy in Varying Skin Pigments
“Racial Effects on Masimo Pulse Oximetry: A Laboratory Study”
Barker SJ, Wilson WC. J of Clin Monit and Comput. 2022;37,567-74.
- The authors concluded that “Masimo RD SET® pulse oximeter sensors showed an absence of clinically significant differences in accuracy between Black and White subjects.”13
“Racial Effects on Masimo Pulse Oximetry: Impact of Low Perfusion Index”
Sharma et al. J Clin Monit and Comput. 2024;38(2):347-354.
- The authors concluded that “Masimo SET® pulse oximeters with RD SET® sensors are accurate for individuals of both Black and White races when Pi [perfusion index] is normal, as well as during conditions when perfusion index is low.”12
-
CLINICAL EVIDENCE
Optimized Screening for Large Populations
“Pulse Oximetry with Clinical Assessment to Screen for Congenital Heart Disease in Neonates in China: A Prospective Study”
Zhao et al. Lancet. 2014 Aug 30;384(9945):747-54.
- The authors concluded that “In the prospective multicentre study, we screened 122,738 consecutive newborn babies (120,707 asymptomatic and 2031 symptomatic), and detected congenital heart disease in 1071 (157 critical and 330 major) […] The addition of [Masimo SET®] pulse oximetry to clinical assessment improved sensitivity for detection of critical congenital heart disease from 77.4% […] to 93.2%…”28
“Experiences From an Implementation Model of ARI Diagnostic Device in Pneumonia Case Management Among Under-5 Children in Peripheral Healthcare Centers in India”
Kumar, H et al. Clin Med Insights Pediatr. 2021. 15:11795565211056649.
- The authors concluded that “The [Masimo SET®] pulse oximeter [was] highly acceptable among health workers as it helped in timely classification and treatment of pneumonia [for 4,846 children].”29
-
CLINICAL EVIDENCE
Reduced Costs While Prioritizing Sustainability
“Impact of Innovative Pulse Oximeter Sensor Management Strategy”
Palmer, A. Biomed Instrum Technol. 2021. 55(2):59-62.
- The author concluded that “The practice of retaping sensors [with Masimo replacement tapes] allows clinicians to recheck and reposition sensor sites frequently with minimal cost and difficulty […] The implementation of [replacement tapes] maximized sensor life and substantially reduced sensor costs and medical waste.”17
Seamless Transition and Support
Bringing SET® into Your Facility

Return on Investment (ROI)
Studies have shown that investing in Masimo SET® has resulted in long-term savings for healthcare facilities.

Saving Lives
- 0 preventable deaths or brain damage due to opioid-induced respiratory depression (OIRD) in over 10 years25
- 80% reduction in rate of retinopathy of prematurity (ROP), an eye disorder that can cause blindness in premature babies23

Saving Time
- 86% fewer false alarms11
- 60% approximate reduction in rapid response team activations26

Saving the Environment
- 60% reduction in single-patient-use sensor utilization17
- 84% reduction in waste with RD SET sensors when compared to cable-based sensors16

Saving Money
- $7M in total cost avoidance over 12 years17
- 50% approximate reduction in unplanned ICU transfers26
Download our information sheet to learn more about how healthcare facilities can save with Masimo.

Whether you are a clinical researcher or a clinician concerned about patient care, it is important to consider proper study methodology to make informed decisions and help advance research.
See how you can help contribute.
Ongoing Support
Masimo provides:
- Hands on educational sessions and seamless implementation ensure minimal disruption to patient care.
- Quick access to clinical experts and technical support teams.
Pulse Oximetry Sensor Application
Need a refresher training on sensor application best practices?
Visit our resource center for pulse oximetry sensor application tips and tricks with step-by-step visuals tailored to your sensor, patient population, and application site.
Masimo SET® Voices

“When we started to look for pulse oximetry technology, we found that the Masimo sensor had a lot of technology for rejecting noise and motion.”
- Susan McGrath, PhD | Associate Professor, Department of Anesthesiology & Director, Patient Surveillance Research & Development, Dartmouth-Hitchcock Medical Center, USA

“Masimo provided us the SET® technology that allows you to continuously monitor the patient from a central device […] we noticed a sharp reduction in false alarms…”
- Professor Thomas Erb | Chief Physician, Anesthesiology/Outpatient Clinic, UKBB University Children’s Hospital, Switzerland
Share Your Masimo SET® Story
Do you have an inspirational story about how Masimo SET® transformed care at your facility or saved a patient’s life?
Resources
Materials
Latest Innovations
Videos
Studies
Contact
Set Up Your Risk-Free Trial
Contact us today for more information on how Masimo SET® can make a difference for your healthcare organization.
Comparative studies include abstracts presented at scientific meetings and peer-reviewed journals. Clinical studies on pulse oximetry and the benefits of Masimo SET® can be found at https:// professional.masimo.com/clinical-evidence.
Estimate: Masimo data on file.
https://www.newsweek.com/rankings/worlds-best-hospitals-2024/united-states.
Masimo RD SET Sensor Instructions for Use: LAB-10131D posted on https://techdocs.masimo.com/.
Hafen, BB. et al. Oxygen Saturation. 2022.
Mayo Clinic. Hypoxemia. Accessed 7/1/2024.
Cellular Respiration. Encyclopedia Britannica. 2023. Accessed: 5/16/2024.
Cleveland Clinic. Hypoxemia. Accessed: 5/16/2024.
Chan ED, et al. Respir Med. 2013;107:789-799.
Shah N et al. J Clin Anesth. 2012 Aug;24(5):385-91.
Hay W et al. J Perinatol. 2002;360–366.
Sharma V, et al. J Clin Monit and Comput. 2024 Jan;38:347-354.
Barker SJ, Wilson WC. J Clin Monit Comput. 2023;37:567-574.
Foglia EE, et al. J Pediatr. 2017 Mar;182:375-377.e2.
Food and Drug Administration (FDA). Pulse Oximeters. – Premarket Notification Submissions Guidance
Masimo data on file.
Palmer, A. Biomed Instrum Technol. 2021. 55(2):59-62.
Masimo OEM Partners found at https://professional.masimo.com/oem/partners/
Baquero H et al. Acta Paediatr. 2011 Apr;100(4):515-8.
Siefkes H, et al. Am J Perinatol. 2020; 37(2):158-165.
Uygur O et al. Pediatr Neonatol. 2019;60(1):68-73.
Schena F et al. J Pediatr. 2017;183:74-79.
Chow LC et al. Pediatrics. 2003;111(2):339-45.
Castillo A et al. Acta Paediatr. 2011 Feb;100(2):188-92.
McGrath S et al. J Patient Saf. 2021; 17(8):557-561.
McGrath S et al. Jt Comm J Qual Patient Saf. 2016; 42(7): 293-302.
Harris B. et al. Ped Crit Care Med. 2016;17(4):315-20.
Zhao Q et al. Lancet. 2014 Aug 30;384(9945):747-54.
Kumar, H et al. Clin Med Insights Pediatr. 2021. 15:11795565211056649.
* ARMS accuracy is a statistical calculation of the difference between device measurements and reference measurements. Approximately two-thirds of the device measurements fell within ± ARMS of the reference measurements in a controlled study.
† Measure through motion and low perfusion parameters.
‡ Fluid responsiveness status in select populations of mechanically ventilated adults. The accuracy in predicting fluid responsiveness is influenced by numerous patient, procedure, and device-related factors and does not measure stroke volume or cardiac output. Fluid management decisions should be based on a complete assessment of the patient’s condition.
PLCO-007370/PLM-11172A-0624